Sathvika Shetty
Senior Consultant (Healthcare, Life Science)
Proactive Worldwide, Inc.
Published: November 2, 2023

In today’s ever-evolving healthcare landscape, the shift towards value-based care models has become imperative. Payers play a crucial role in driving this transformation as the focus moves from quantity to quality. This article by Proactive Worldwide aims to provide insights and strategies tailored specifically for payers. It seeks to empower payers to successfully implement value-based care initiatives while also highlighting how competitive intelligence can support this endeavor.
Understanding Value-Based Care (VBC)
VBC is a healthcare delivery model that prioritizes the overall value of care delivered to patients, rather than simply the volume of services provided. It emphasizes delivering high-quality care, improving patient outcomes, and reducing healthcare costs. This approach aims to shift the focus from fee-for-service reimbursement towards incentivizing providers based on the quality and effectiveness of their care.
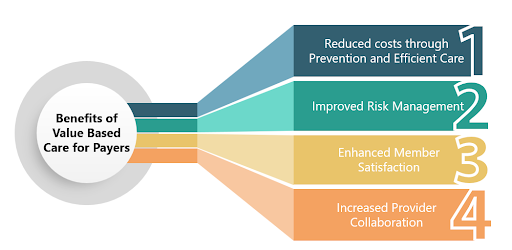
Benefits of VBC for Payers
VBC offers health insurance companies a multitude of benefits, including reduced costs through prevention and efficient care, improved risk management, enhanced member satisfaction, and increased provider collaboration.
Implementation Challenges
Transitioning to value-based care comes with a lot of challenges that need to be addressed. Some of the challenges have been listed below:
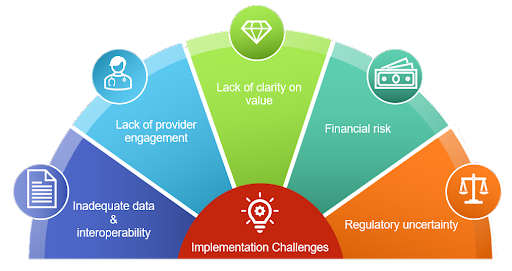
- Inadequate data and interoperability: VBC requires access to accurate and reliable data on patient health outcomes, costs, and utilization. Unfortunately, this is often hindered by the ongoing challenges related to data sharing between payers and providers. Incompatibilities in systems and data formats create barriers that impede efficient and seamless data exchange.
- Lack of provider engagement: Payers need the buy-in and participation of providers to successfully implement VBC. However, some providers may be reluctant to adopt VBC due to concerns such as apprehensions about increased administrative workload, financial risks, or insufficient understanding or trust in the concept.
- Lack of clarity on value: Value in healthcare lacks a universally accepted definition, resulting in varying perspectives among stakeholders regarding its core components. This can present challenges for both payers and providers to agree on the goals and metrics for VBC programs. The absence of a standardized understanding of VBC poses complexities in achieving alignment and collaborative decision-making.
- Financial risk: VBC programs often involve shared financial risk between payers and providers. However, this can pose challenges for payers as they are exposed to potential financial losses if providers fail to achieve the desired outcomes.
- Regulatory uncertainty: The regulatory framework surrounding VBC is in a state of constant change, contributing to an air of uncertainty for both payers and providers. The ever-changing regulatory environment can pose challenges as stakeholders navigate the intricate requirements of VBC.
Strategies for Implementing Value-Based Care
Despite these challenges, there is a growing momentum towards VBC to improve the quality and value of care. Payers who can overcome these challenges can reap significant benefits, including lower costs, improved patient outcomes, and increased satisfaction. To successfully implement value-based care, health insurance companies might consider the following strategies:
- Provider Engagement and Education: Fostering active engagement and facilitating education among healthcare providers are crucial steps in successfully implementing VBC. This includes comprehensive educational initiatives like training programs, workshops, and collaborative forums to ensure alignment between payers and providers.
- Data Analytics and Performance Measurement: Leverage advanced data analytics to gather, analyze, and interpret healthcare data for effective VBC implementation. This enables insurers to identify key quality metrics, track patient outcomes, and accurately measure provider performance. By harnessing the potential of data analytics and performance measurement, stakeholders can unlock valuable insights and drive positive transformations in the healthcare landscape.
- Alternative Payment Models: Introduce alternative payment models, such as bundled payments or shared savings arrangements, which can reform the healthcare landscape to align financial incentives with quality outcomes. This encourages providers to focus on delivering efficient, coordinated, and patient-centered care. Alternative payment models promote a value-based approach that rewards successful outcomes rather than simply paying for services rendered. By providing financial incentives that align with quality, stakeholders can foster a healthcare system that prioritizes value, enhances patient experiences, and drives improved health outcomes.
- Care Coordination and Population Health Management: Implement effective care coordination programs that facilitate provider collaboration and communication. This helps to ensure seamless transitions of care and promotes preventive measures, ultimately improving population health. This paves the way for improved patient experiences, optimized health outcomes, and a more holistic approach to healthcare delivery.
- Incentivizing Value-Based Care: To foster the adoption of VBC, it is crucial to design payment structures that incentivize providers based on value and outcomes, rather than the volume of services rendered. This could be achieved through shared savings programs, pay-for-performance models, or performance-based bonuses.
- Patient Engagement and Empowerment: Promote patient engagement by providing tools and resources that encourage proactive involvement of patients in their own healthcare journey. This could involve health coaching, readily accessible patient education materials, and innovative technological solutions for remote monitoring and self-management. By fostering patient engagement, stakeholders can enable individuals to make informed decisions, take control of their health and actively participate in their care.
How Can Proactive Worldwide Help?
Proactive Worldwide is a leading specialty market research firm providing market and customer intelligence that can leverage competitive analysis to provide in-depth insights into the market landscape, industry trends, and competitor strategies shaping the VBC landscape. Some ways Proactive Worldwide can support the implementation of value-based care include:
- Market Analysis: Helps payers understand the market dynamics, including competitor offerings, strategies, and market share. This information enables insurers to identify gaps in the market and design value-based care strategies that differentiate their offerings and align with market demands.
- Identifying Best Practices: Competitive intelligence allows payers to learn from the best practices implemented by industry leaders and successful VBC organizations. By analyzing competitor strategies, payers can identify innovative care models, successful reimbursement structures, and effective provider engagement approaches for their implementation.
- Benchmarking Performance: Provide payers with comparative data to benchmark performance against competitors. Payers can evaluate their performance in terms of patient outcomes, cost control, care coordination, and provider networks. This comparison allows them to identify areas for improvement and develop strategies to outperform competitors in delivering value-based care.
- Tracking Industry Trends: Proactive Worldwide can help payers stay abreast with the latest trends in VBC. This includes monitoring regulatory changes, payment reforms, new reimbursement models, and emerging technologies through our customizable newsletters. Staying informed about industry trends ensures that insurers can adapt and evolve their VBC strategies to align with the changing healthcare landscape.
- Partnership Opportunities: Enables payers to identify potential strategic partnerships and collaborations. By analyzing competitors’ affiliations with healthcare organizations, accountable care organizations (ACOs), or integrated delivery networks (IDNs), insurers can identify partnership opportunities that enhance care coordination, improve outcomes, and drive value-based care initiatives.
- Insights into Provider Network: Competitive intelligence provides insights into competitors’ provider networks, including relationships with hospitals, specialists, and other healthcare facilities. This information helps payers formulate strategies to improve their provider network by recruiting high-performing providers, ensuring adequate geographic coverage, and fostering collaborative relationships with key healthcare partners.
Conclusion
Proactive Worldwide empowers health insurance companies with the knowledge needed to make informed decisions and implement effective value-based care models. By leveraging market analysis, benchmarking, trend monitoring, and partnership insights, insurers can develop competitive strategies that drive positive patient outcomes, cost savings, and successful implementation of value-based care initiatives.